In a recent survey of more than 27,000 cancer patients, a remarkable 73.8% reported that their telehealth visits were as good or better than in-person consultations. The study, which ran from May 2020 to October 2023, highlights a significant shift in patient satisfaction with telehealth services, especially as the pandemic accelerated its adoption.
By 2023, only 18.9% of respondents felt that telehealth was worse than traditional visits, a sharp contrast to 31% in 2020. Additionally, an impressive 90.3% of patients expressed a preference for telehealth visits in the future, indicating strong support for this method of care.
However, not all experiences are equal. A parallel study revealed stark racial disparities in perceptions of telehealth’s effectiveness and accessibility. Among the 773 cancer patients surveyed, 42% identified as Black, and they reported lower digital literacy and trust in healthcare providers compared to their non-Black counterparts.
Notably, 48% of Black respondents doubted the usefulness of telehealth for assessing health needs, compared to 37% of non-Black patients. These findings underscore the urgent need for cancer care practices to enhance communication strategies and address the specific concerns of diverse patient populations.
As we navigate this evolving landscape of cancer care, it becomes increasingly clear that while telehealth offers substantial benefits, tailored approaches are essential to ensure equitable access and satisfaction for all patients.
Understanding Telehealth in Cancer Care
In a world where nearly two million people in the United States are diagnosed with cancer each year, the integration of telehealth into cancer care—often referred to as tele-oncology—has emerged as a transformative approach. Take the Johnson family, for instance.
When their daughter Mia was diagnosed with advanced Wilms tumor at just seven years old, they faced the daunting task of traveling two and a half hours to seek expert advice. Instead of making that journey, they opted for a video consultation with a pediatric oncologist at Cancer Center. This choice not only saved them time but also allowed them to stay in the comfort of their home during a challenging period.
Sarah Johnson shared how this virtual visit made a significant difference: “When your child is going through cancer, just those little things—like you get to stay home one more day instead of having to go to the hospital again—can make a big difference.”
The oncologist reviewed Mia’s medical history and discussed treatment options, all from their kitchen table. This convenience extended to subsequent consultations with other specialists, allowing the family to coordinate Mia’s care seamlessly.
Telehealth offers numerous advantages for cancer patients and their families: reduced travel costs, flexible scheduling, and lower exposure to germs for immunocompromised individuals. While it cannot completely replace in-person care, it reshapes the cancer care experience, making it more accessible and less burdensome.
As telehealth continues to evolve, experts emphasize the need for ongoing research to ensure equitable access and integration into standard cancer care practices.
How Race Affects Cancer Patients’ Experience with Telehealth
The COVID-19 pandemic accelerated the adoption of telehealth, offering a lifeline to many patients who could not easily access in-person care.
However, disparities in access to technology & the internet have emerged, particularly affecting racial minorities. For instance, a study revealed that Black patients were significantly less likely to participate in telehealth visits compared to their White counterparts.
While Black patients made up 43% of total visits at a cancer center, only 29% of telehealth consultations involved them. This stark contrast highlights underlying systemic issues that need addressing.
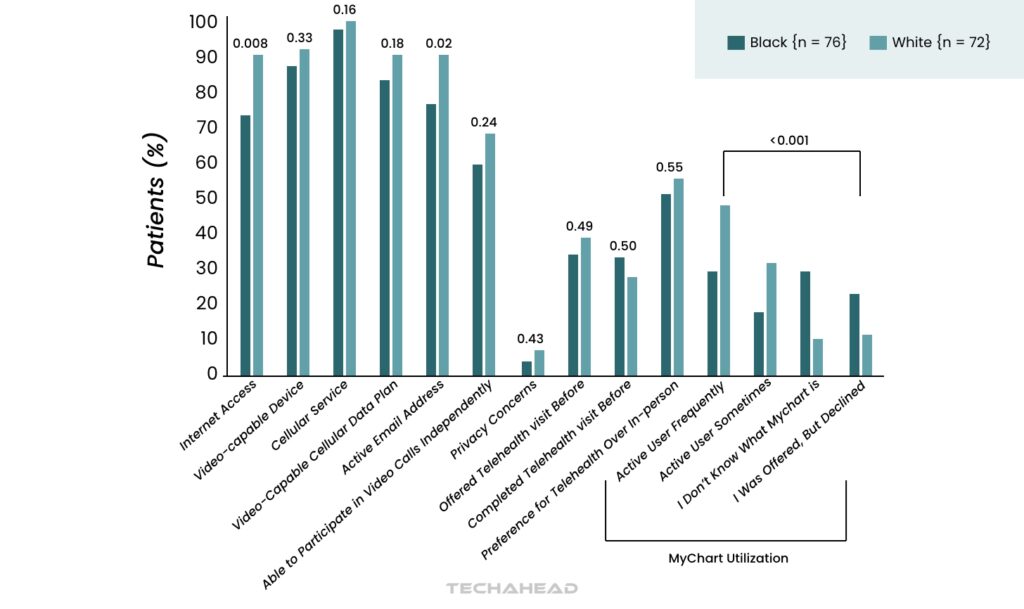
Access to reliable internet is one of the primary barriers faced by many Black patients. In fact, a staggering 73.7% of Black participants reported lacking adequate internet access, compared to just 9.6% of White patients. This digital divide can severely limit their ability to engage in telehealth services, which are increasingly vital for managing chronic conditions like cancer.
Furthermore, Black patients reported lower rates of using patient portals—tools that facilitate communication with healthcare providers—compared to their White peers. Only 29% of Black participants actively used such portals, compared to 47% of White participants.
The implications of these disparities extend beyond mere convenience; they can impact health outcomes and the overall quality of care received by racial minorities. Telehealth is designed to reduce barriers such as travel costs and time away from work or family responsibilities, making it an ideal solution for many.
However, if certain populations cannot access these services due to technological limitations, the potential benefits are lost.
In addition to internet access, factors like digital literacy and comfort with technology play significant roles in a patient’s ability to utilize telehealth effectively.
Many older adults or individuals from disadvantaged backgrounds may struggle with navigating digital platforms, further exacerbating disparities in care. This lack of familiarity can lead to feelings of frustration and isolation during an already challenging time.
Moreover, the socioeconomic status of patients cannot be overlooked when discussing access to telehealth. Many Black patients reported lower household incomes compared to White patients, which can affect their ability to afford necessary technology or reliable internet service.
For instance, nearly half of the Black participants surveyed reported a household income below $20,000 or relied on disability benefits, a stark contrast to their White counterparts.
Addressing these disparities requires a multifaceted approach that includes improving internet infrastructure in underserved communities and providing education on how to use telehealth technologies effectively. Healthcare providers must also be aware of these challenges and work proactively to ensure that all patients have equal access to telehealth services.
As we move forward in integrating telehealth into cancer care, it’s essential that we consider these racial disparities seriously. Ensuring equitable access will not only improve individual patient experiences but also contribute to better health outcomes across diverse populations.
By recognizing and addressing the barriers faced by racial minorities in accessing telehealth, we can take meaningful steps toward achieving health equity for all cancer patients. The journey toward equitable healthcare is ongoing, but understanding how race affects patient experiences with telehealth is a critical step in this important endeavor.
Addressing the Gaps in Telehealth for Diverse Cancer Patients
For instance, studies have shown that Black patients are disproportionately less likely to utilize telehealth services compared to their White counterparts. While Black patients made up 43% of total visits at a regional cancer center, only 29% of telehealth consultations involved them, raising concerns about equitable access to this crucial resource.
One of the primary barriers contributing to this disparity is reliable internet access. Many Black patients report lacking sufficient internet connectivity, which hinders their ability to participate in virtual appointments.
In fact, a staggering 73.7% of Black participants in one study indicated they did not have reliable internet access, compared to only 9.6% of White patients. This digital divide not only limits access to telehealth but also exacerbates existing health disparities, as those who need care the most may be unable to receive it.
Digital literacy is another significant factor affecting telehealth utilization among diverse cancer patients. Many individuals from socially disadvantaged backgrounds may struggle with navigating technology or feel uncomfortable using virtual platforms for medical consultations.
This lack of familiarity can lead to frustration and anxiety, making it less likely that they will seek out or engage with telehealth services. Moreover, the socioeconomic status of these patients often plays a role; lower-income households may not have the resources to invest in necessary technology or high-speed internet service.
To effectively address these gaps, healthcare providers and policymakers must prioritize equitable access to telehealth services. This includes investing in infrastructure improvements in underserved communities to ensure all patients have reliable internet access.
Additionally, educational initiatives aimed at improving digital literacy can empower patients to navigate telehealth platforms confidently. By providing training sessions or resources on how to use telehealth technologies, healthcare systems can help bridge the gap between those who are comfortable with technology and those who are not.
Furthermore, healthcare organizations should consider implementing policies that specifically target the needs of diverse populations. This could include offering telehealth services in multiple languages or providing culturally competent care that acknowledges and respects the unique experiences of different racial and ethnic groups.
Engaging community leaders and organizations can also help raise awareness about available telehealth services and encourage participation among minority populations.
Another critical aspect of improving telehealth for diverse cancer patients is ensuring that healthcare providers are trained to recognize and address the unique barriers faced by their patients.
By fostering an environment of understanding and support, providers can help alleviate some of the concerns that may prevent patients from utilizing telehealth services. Regular feedback from patients about their experiences with telehealth can also inform ongoing improvements and adaptations to better meet their needs.
As we continue to integrate telehealth into cancer care, it is vital to remain vigilant about addressing these disparities. Ensuring equitable access will not only enhance individual patient experiences but also contribute to better health outcomes across diverse populations.
By recognizing and addressing the barriers faced by racial minorities in accessing telehealth, we can take meaningful steps toward achieving health equity for all cancer patients. The journey toward equitable healthcare is ongoing, but by focusing on these critical areas, we can create a more inclusive system that serves everyone effectively.
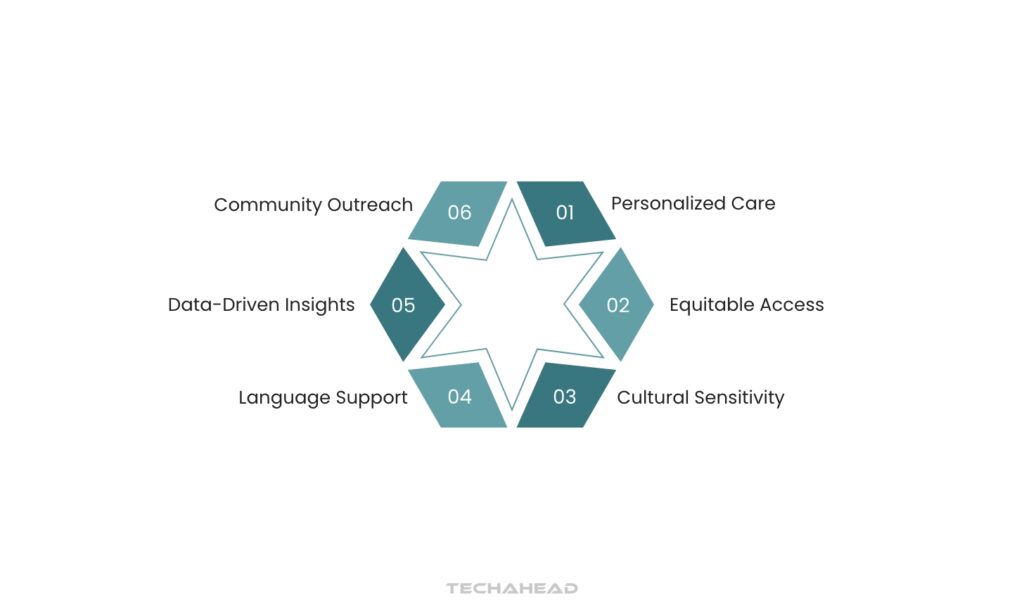
Strategies for Improvement
Understanding and addressing differences is crucial for creating a more equitable healthcare system that provides high-quality, compassionate care to all patients, regardless of their racial background. By adopting these strategies, healthcare systems can work towards more inclusive, patient-centered telehealth experiences that genuinely serve the diverse needs of cancer patients across all racial backgrounds.
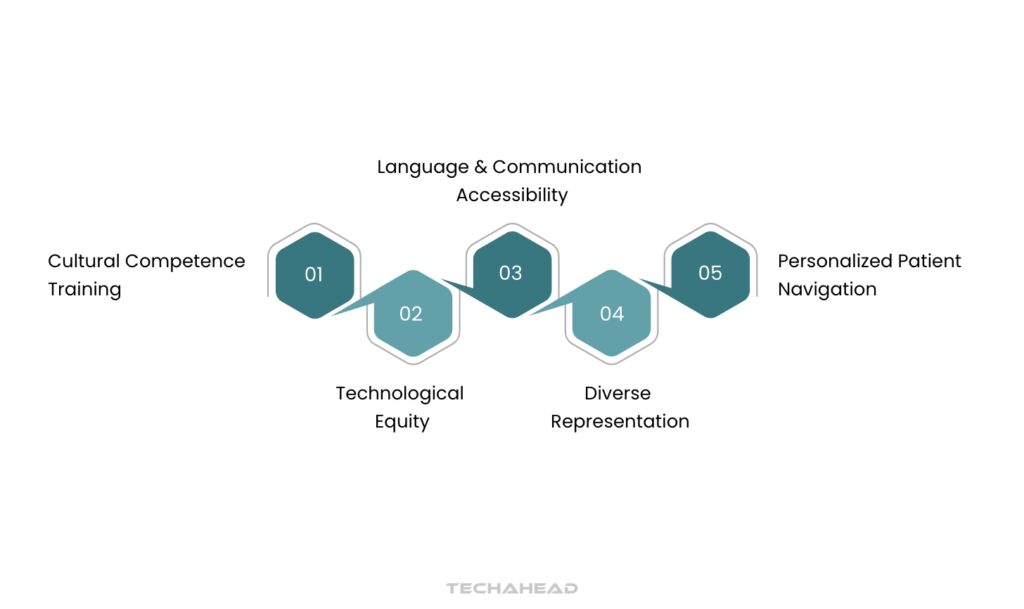
Cultural Competence Training
First of all for telehealth to truly serve diverse populations, healthcare providers need more than just medical expertise. They require comprehensive training that emphasizes cultural sensitivity and effective communication.
This training should delve into understanding the nuances of different cultures, recognizing and mitigating unconscious biases, and mastering communication techniques that acknowledge and respect each patient’s unique cultural background. This goes beyond simply knowing facts about a culture; it’s about developing genuine empathy and understanding.
By fostering a healthcare environment where patients feel seen, heard, and respected, providers can build stronger therapeutic relationships and increase patient comfort during virtual interactions. This, in turn, leads to better health outcomes and a more equitable healthcare experience for all.
Language & Communication Accessibility
Secondly, breaking down language barriers is crucial for equitable healthcare access in our increasingly diverse world. Investing in professional translation and interpretation services is essential. This means more than just automated translations; it requires skilled human interpreters who understand medical terminology and cultural nuances.
Furthermore, telehealth platforms should be designed with multilingual capabilities from the outset. This includes offering interfaces, instructions, and educational materials in multiple languages.
By ensuring seamless communication between patients and providers, we can avoid misunderstandings that can lead to misdiagnosis, incorrect treatment plans, and ultimately, poorer health outcomes. This investment not only improves patient satisfaction but also enhances the quality and safety of care for everyone.
Technological Equity
Also, bridging the digital divide is crucial for equitable telehealth access. Recognizing that reliable internet and device access differs significantly across racial and socioeconomic groups, targeted programs are essential. These programs should go beyond simply offering telehealth services and actively address the technological barriers patients face.
One key strategy is providing technology support. This could include loaning devices like tablets or laptops to patients who lack them. Offering internet subsidies or connecting patients with existing low-cost internet programs can also significantly improve access. Furthermore, designing simplified, user-friendly interfaces is crucial.
These interfaces should be intuitive for individuals with varying levels of technical skills, ensuring that everyone can easily navigate telehealth platforms and participate in their care. By proactively addressing these technological challenges, healthcare providers can ensure that telehealth reaches all patients, regardless of their background.
Personalized Patient Navigation
Next, to address disparities in cancer care, implementing patient navigation programs tailored to racial minority groups is crucial. These programs offer personalized support to help patients navigate the complexities of the healthcare system. Patient navigators act as guides, assisting with various aspects of the cancer journey.
They explain treatment options in clear, understandable terms, help schedule appointments with specialists, and connect patients with resources to overcome logistical hurdles like transportation or financial assistance.
Crucially, they also provide emotional support, addressing the anxieties and uncertainties that often accompany a cancer diagnosis. By offering culturally sensitive support and addressing the unique needs of diverse patient populations, these programs can significantly improve access to care, treatment adherence, and ultimately, patient outcomes.
Diverse Representation
Ultimately, for telehealth to be truly equitable, it’s essential to increase racial diversity among providers and support staff. Patients often experience greater comfort and a stronger sense of connection when their healthcare team shares their background.
This sense of connection fosters trust and open communication, leading to improved patient satisfaction and better adherence to treatment plans. Currently, many healthcare settings lack this crucial representation, creating a barrier for patients from diverse racial and ethnic groups.
By actively recruiting and supporting individuals from underrepresented communities in healthcare professions, we can build a more inclusive and culturally competent telehealth workforce. This not only benefits patients but also enriches the healthcare system with diverse perspectives and experiences, ultimately leading to better health outcomes for all.
The Future of Telehealth in Cancer Care for All Races
From a clinician’s perspective, much of the data on telemedicine’s impact comes from surveys conducted early in the pandemic. These surveys revealed that while telemedicine occasionally led to urgent in-person visits, unplanned diagnostic studies, and medication adjustments, adverse outcomes directly attributable to telemedicine were rare.
Many providers expressed an intent to continue using telemedicine for certain types of visits, but actual adoption rates have been lower than initially projected. This discrepancy raises questions about the influence of regulatory uncertainties, integration challenges, and patient preferences.
Patient satisfaction with telemedicine has been varied. While some studies indicated a preference for returning to in-person visits post-pandemic, others showed high satisfaction rates with the telemedicine experience. The suitability of telemedicine depends heavily on the specific patient population and their individual circumstances.
For example, patients with head and neck cancers, often facing communication challenges, may find telemedicine less effective.
Several challenges hinder the widespread and equitable implementation of telemedicine. These include the need for more robust data on outcomes, particularly regarding emergency department visits.
Increased focus is needed on patient and clinician education about the appropriate use of telemedicine, along with training on the technology itself. Privacy and confidentiality concerns, including regulatory protections for providers, and the role of local clinics also require attention.
Perhaps the most pressing issue is the digital divide. Factors such as age, rural residence, race, ethnicity, and socioeconomic status are significantly associated with access to telemedicine. Disparities in broadband access, device ownership, and digital literacy further exacerbate this divide.
It’s crucial to acknowledge that not all patients can or want to participate in telemedicine, and healthcare systems must develop resilient workflows to accommodate their diverse needs and preferences.
From a policy standpoint, while the pandemic prompted temporary waivers expanding Medicare telehealth access, the future of these flexibilities remains uncertain. Cross-state licensure, requiring physicians to obtain multiple licenses, presents another barrier.
Payers, too, are playing a crucial role in shaping the future of telemedicine. Many have expressed a commitment to continuing support & reimbursement for telehealth across various specialties. While utilization has decreased from its pandemic peak, it remains significantly higher than pre-pandemic levels, indicating a sustained demand for virtual care.
Payers recognize the need to address the digital divide and ensure equitable access to telehealth. They are also exploring innovative programs, such as virtual centers of excellence and enhanced support programs, to improve the quality and accessibility of cancer care through telemedicine.
The future of telehealth in cancer care hinges on addressing these challenges & maximizing the opportunities it presents. This includes gathering more data on outcomes, improving patient & provider education, bridging the digital divide, and establishing clear policies and reimbursement models.
By focusing on these areas, we can ensure that telemedicine becomes a valuable tool for expanding access to high-quality cancer care for all populations, regardless of race, ethnicity, or socioeconomic status.
FAQ
Telehealth has the potential to break down barriers such as geographic isolation and transportation challenges, enabling underserved communities, including racial minorities, to receive timely medical care without needing to travel outside their neighborhoods. This innovative approach allows patients to connect with healthcare providers remotely, ensuring they have access to the consultations and support they need while remaining close to home.
Elderly patients often encounter challenges that can affect their satisfaction with telehealth services. Many may not be familiar with technology, making it difficult for them to use devices effectively. Additionally, issues like poor internet connectivity can further complicate their experience, leading to frustration and dissatisfaction with virtual healthcare options. Addressing these barriers is essential for improving telehealth accessibility for older adults.
Patients from lower socioeconomic backgrounds often struggle with limited access to high-speed internet, smartphones, or computers. This lack of resources can hinder their ability to fully engage with telehealth services, leading to lower levels of satisfaction. Addressing these challenges is essential to ensure that all patients can benefit from telehealth, regardless of their economic situation.