In the intricate landscape of modern healthcare, administrative inefficiencies are silently eroding the potential for transformative patient care. The healthcare and life sciences industry is undergoing a digital transformation, driven by technological advancements & increasing patient expectations.
According to Gartner, a significant surge in IT spending in the healthcare sector, with a projected growth of 9.5% in 2024, reaching a staggering $265.2 billion. This trend is fueled by a growing emphasis on IT services and software, with expected annual growth rates of 10.4% and 13.4%, respectively.
Imagine a typical doctor’s office: a receptionist navigating through stacks of paperwork, manually scheduling appointments, and entering patient data—each keystroke representing a potential point of human error. These repetitive tasks not only consume valuable time but also divert healthcare professionals’ attention from what truly matters—patient care.
As the healthcare industry stands at a critical crossroads, the integration of digital process automation emerges as a beacon of hope, promising to streamline operations, reduce expenses, and ultimately improve the affected person’s experience. The future of healthcare isn’t always pretty much technological development; it’s approximately reimagining how we deliver care.
Key Takeaways:
- Healthcare organizations must embrace digital technologies to improve patient experience, streamline operations, and drive innovation.
- Prioritizing patient needs and preferences is essential for long-term success.
- Healthcare organizations must be agile and adaptable to changing market dynamics and emerging technologies.
Critical Decisions Shaping the Future of Healthcare Deliver
In the rapidly evolving landscape of healthcare, significant transformations are anticipated by 2030, driven by various factors that prioritize patient-centric care and efficiency. TechAhead’s extensive research, which included over 50 interviews with healthcare executives and industry experts, highlights several key areas poised for disruption in the coming decade.
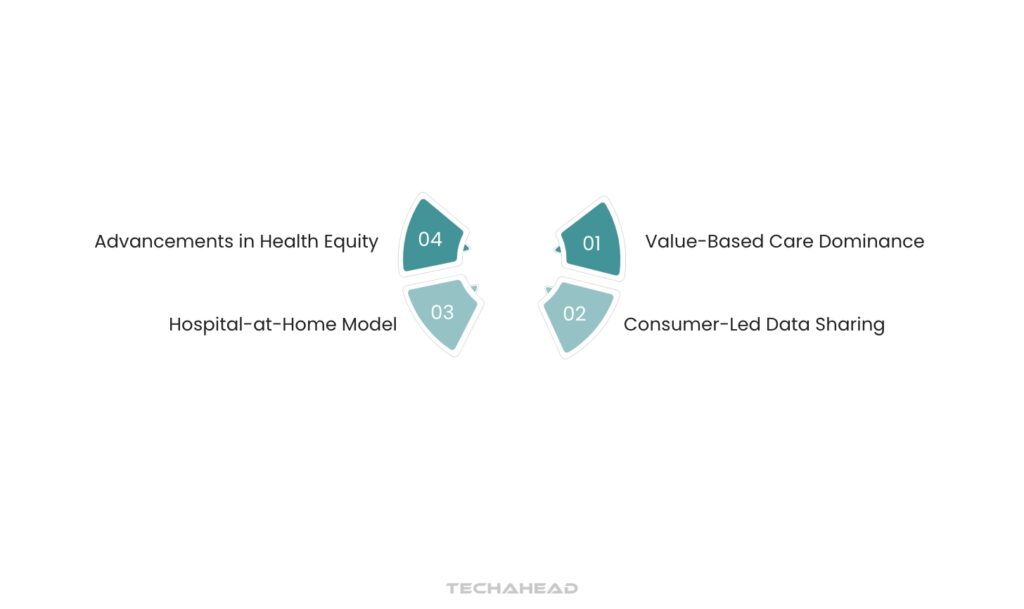
Value-Based Care Dominance
One of the most notable shifts will be the transition to value-based care (VBC) as the primary reimbursement model. This approach emphasizes preemptive and home-based care, allowing healthcare organizations (HCOs) to take on greater financial risks associated with patient outcomes.
As consumers demand more cost transparency, HCOs will need to adopt episodic care models that provide upfront cost estimates for services. Success in this area hinges on developing robust metrics that hold both patients and clinicians accountable for their roles in the care process.
Consumer-Led Data Sharing
As we move towards a more democratized healthcare system, consumer-led data sharing will gain traction. By 2030, patients will have greater control over their health data, determining who can access it and under what conditions.
This evolution is driven by regulatory changes like the Cures Act Final Rule, which mandates improved data portability across healthcare platforms. Institutions that resist this trend risk obsolescence as consumers increasingly demand transparency and accessibility regarding their health information.
Hospital-at-Home Model
The concept of hospital-at-home is set to redefine where and how care is delivered. By 2030, it is expected that patients will primarily receive care in their homes, reserving traditional hospital settings for only the most invasive procedures or when home conditions are unsuitable for treatment.
This shift not only enhances patient comfort but also significantly reduces the utilization of physical hospital resources, leading to a potential wave of clinic closures. Health insurers are likely to respond by acquiring these facilities to manage costs effectively. Projections indicate that by 2029, nearly 29% of evaluation and management visits will occur virtually.
Advancements in Health Equity
The pursuit of health equity will also be a critical focus in the coming years. Achieving optimal health for all individuals requires dismantling systemic barriers that have historically marginalized certain populations. By leveraging representative data sets and advanced analytics within VBC frameworks, HCOs can implement best-practice protocols that ensure equitable access to quality care across diverse communities.
Strategic Actions for HCOs to Navigate Future Healthcare Challenges
Embed Cybersecurity Measures
With an interconnected healthcare ecosystem comes heightened cybersecurity risks. Organizations must adopt a Zero Trust architecture to safeguard sensitive patient data continuously.
Protect Data Value
As the importance of health data escalates, HCOs must prioritize its security and privacy to maintain consumer trust and competitive advantage. Key questions regarding data usage and protection should guide organizational strategies.
Explore New Revenue Streams
Embracing low-acuity care settings can open new revenue opportunities while reducing barriers to technology adoption. Remote patient monitoring is one area where innovative solutions can enhance financial outcomes within both fee-for-service and value-based models.
7 Major Shifts Driven by Digital Transformation Maturity in Healthcare by 2030

The digital transformation of healthcare is set to drive significant changes by 2030, reshaping how care is delivered and experienced. This transformation will be characterized by seven major shifts that prioritize consumer empowerment, trust, inclusivity, value-based payment models, partnerships for better health outcomes, enhanced diagnostic capabilities, and improved health equity.
Consumer Control of Data Will Fuel a New Economy for Healthcare
As patients increasingly demand control over their health data, a new economy will emerge within healthcare. By 2030, consumers are expected to hold the rights to their personal health information, allowing them to dictate how and when their data is shared. This shift will foster a more transparent relationship between healthcare providers and patients, as organizations adapt to meet consumer expectations for privacy and data usage.
The Office of the National Coordinator for Health Information Technology’s Cures Act Final Rule is paving the way for this change by mandating that healthcare data be portable and accessible through consumer-facing applications. This democratization of data will not only empower patients but also drive innovation in healthcare delivery models.
Loyalty in Healthcare Will Require Consumer Trust and Confidence
In an era where choices abound, healthcare organizations (HCOs) must cultivate trust to foster patient loyalty. As consumers become more discerning about their healthcare options, they will gravitate towards providers who demonstrate transparency, reliability, and empathy.
Trust will be built through consistent communication, quality care delivery, and the protection of personal health information. HCOs that prioritize patient engagement and satisfaction will not only enhance loyalty but also improve overall health outcomes. The ability to build a trustworthy relationship with patients will be crucial in retaining them in an increasingly competitive market.
Inclusive Cultures and Empathetic Experiences Will Finally Put the Patient at the Center
The future of healthcare will see a shift towards more inclusive cultures that prioritize empathetic patient experiences. By 2030, HCOs are expected to adopt practices that recognize the diverse needs of their patient populations, ensuring that care is accessible and tailored to individual circumstances.
This approach involves actively listening to patients’ concerns and preferences while incorporating their feedback into care protocols. The emphasis on patient-centered care will not only enhance satisfaction but also lead to better adherence to treatment plans and improved health outcomes.
Value-Based Payment Will Deliver Relief for Clinicians and Consumers
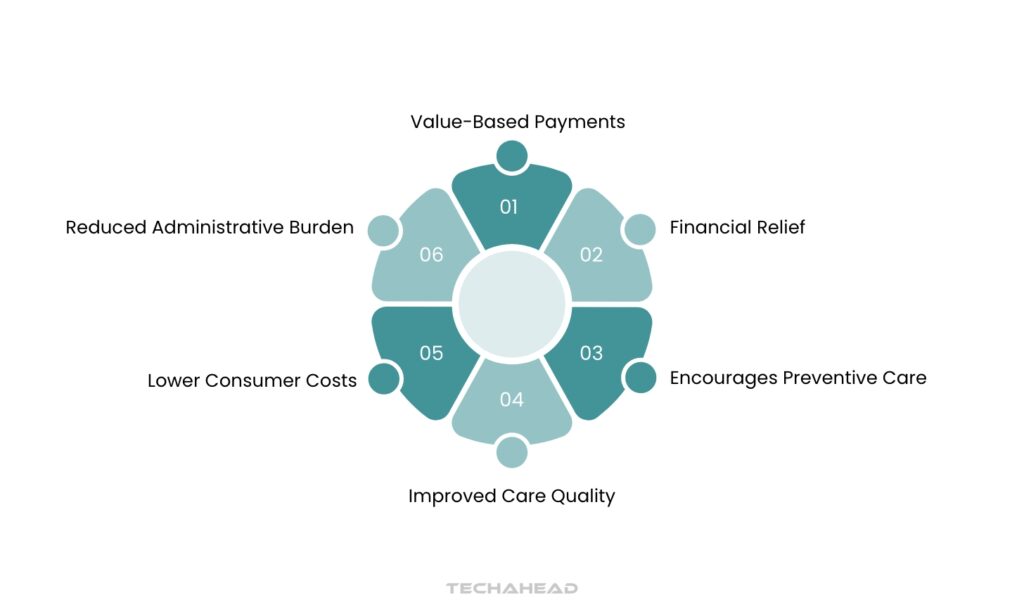
The transition to value-based payment models is anticipated to alleviate some of the financial pressures faced by both clinicians and consumers. By focusing on patient outcomes rather than the volume of services rendered, this model encourages HCOs to invest in preventive care and chronic disease management strategies.
As clinicians are rewarded for delivering high-quality care rather than simply increasing service volume, they can spend more time with patients and less time navigating administrative burdens. This shift not only benefits providers but also results in lower out-of-pocket costs for consumers as care becomes more efficient.
Partnerships Will Deliver Preemptive and Prescriptive Care That Improves Population Health
Collaboration among diverse stakeholders in the healthcare ecosystem is essential for developing comprehensive solutions that effectively address population health needs. By forging partnerships between healthcare organizations (HCOs), technology vendors, insurers, and community organizations, the industry can create innovative preemptive and prescriptive care models aimed at preventing illnesses before they arise.
Utilizing shared data and resources allows these partnerships to identify at-risk populations and implement targeted interventions, ultimately enhancing overall community health outcomes and fostering a proactive approach to healthcare delivery. This collaborative effort is vital for addressing the complexities of modern healthcare and ensuring equitable access to quality care for all individuals.
Digital Health Maturity Will Enable Proactive and Unbiased Diagnosis
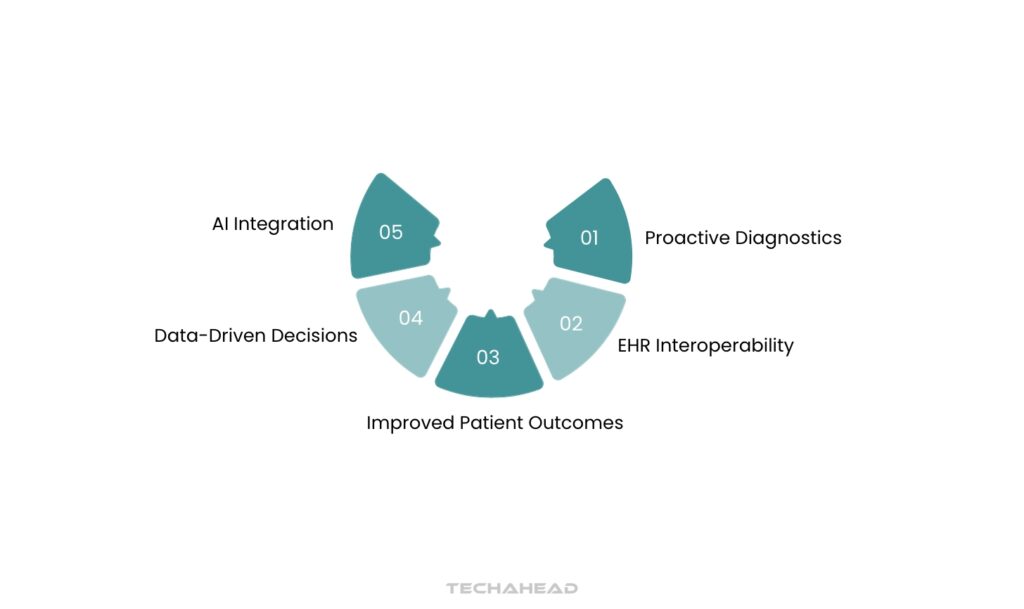
As healthcare organizations advance in their digital maturity, they will be better equipped to deliver proactive and unbiased diagnostic services. Enhanced interoperability among electronic health records (EHRs) will allow clinicians access to comprehensive patient histories, enabling them to make informed decisions based on complete data sets rather than fragmented information.
The integration of artificial intelligence (AI) tools into diagnostic processes can further enhance accuracy by identifying patterns that may not be immediately apparent to human practitioners. This evolution towards data-driven decision-making is expected to reduce diagnostic errors and improve patient safety.
Increased Distribution of Best-in-Class Care Will Improve Health Equity
Finally, the distribution of best-in-class care across diverse populations is crucial for advancing health equity by 2030. Healthcare organizations must actively work to dismantle barriers that prevent marginalized communities from accessing quality care.
This includes expanding access to telehealth services, improving transportation options for in-person visits, and ensuring culturally competent care practices are implemented throughout the system. By utilizing analytics to identify disparities in care delivery and outcomes, HCOs can develop targeted strategies that promote equitable access to high-quality healthcare services.
Key Steps to Prepare Your Organization for 2030
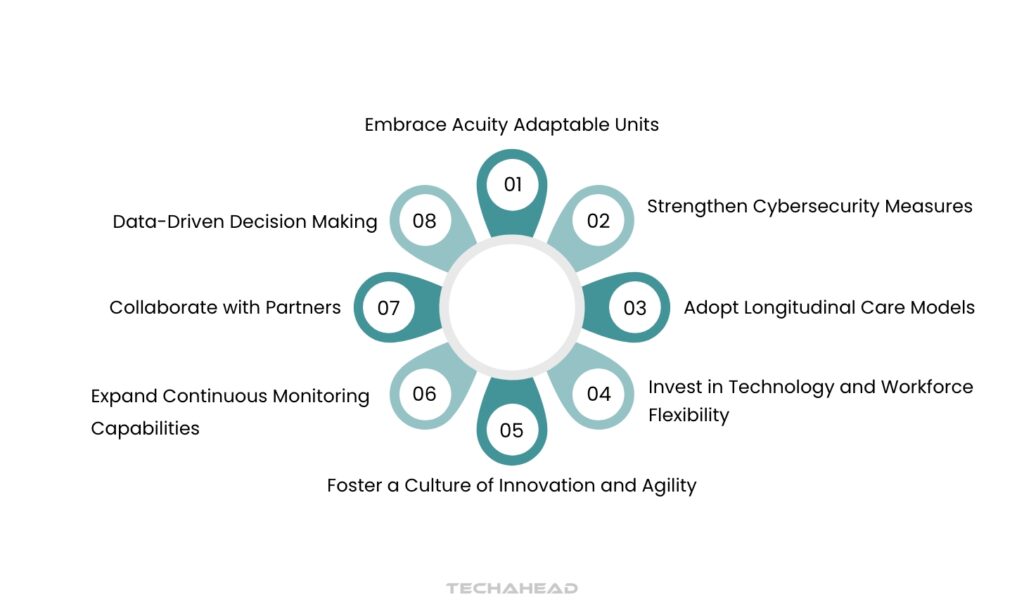
To navigate the complexities of the healthcare landscape in 2030 and beyond, consider these key steps:
Embrace Acuity Adaptable Units
Modular patient room infrastructure with smart sensor-enabled morphing capabilities, dynamically reconfiguring spatial layouts, medical equipment integration, and real-time environmental adaptations to optimize clinical workflow efficiency.
Expand Continuous Monitoring Capabilities
Advanced telemetry and IoT healthcare technologies enable proactive remote patient monitoring, facilitating predictive diagnostics, early clinical interventions, and optimized patient trajectory management with reduced hospitalization duration.
Adopt Longitudinal Care Models
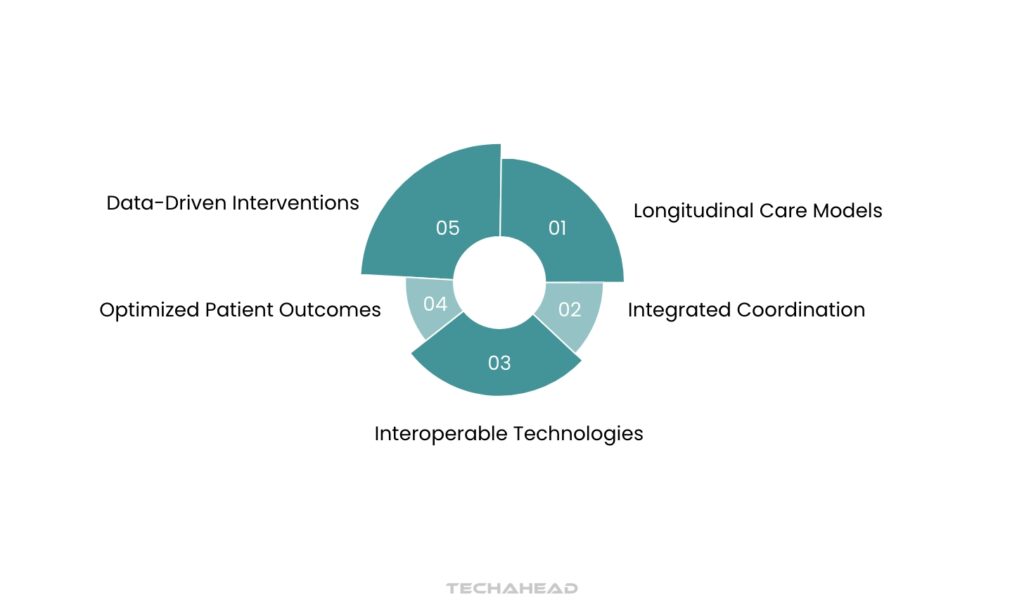
Implement integrated care coordination mechanisms leveraging interoperable healthcare technologies to optimize patient outcomes, enhance cross-setting continuity, minimize readmission risks, and systematically improve overall patient experience through seamless clinical communication and data-driven intervention strategies.
Invest in Technology and Workforce Flexibility
Implement strategic technology modernization and comprehensive workforce upskilling to enhance organizational resilience, enabling agile response to evolving technological and operational landscapes.
Foster a Culture of Innovation and Agility
Foster an adaptive ecosystem that systematically empowers innovation, validates experimental approaches, and drives iterative organizational evolution through data-driven learning and agile methodological frameworks.
Strengthen Cybersecurity Measures
Implement advanced cybersecurity protocols to safeguard sensitive healthcare information management systems, ensuring comprehensive digital infrastructure protection against evolving cyber threats and unauthorized access.
Collaborate with Partners
Implement strategic cross-sector partnerships leveraging interoperable digital platforms to facilitate knowledge exchange, resource optimization, and collaborative healthcare innovation across provider networks, technology ecosystems, and community stakeholders.
Data-Driven Decision Making
Utilize advanced predictive analytics and machine learning algorithms to extract actionable insights from complex healthcare datasets, enabling strategic operational optimization, precision resource allocation, and data-driven patient care enhancement.
Wrapping Up
As we look toward the next decade, the evolution of U.S. healthcare is set to become increasingly preemptive, driven by vast amounts of data, advanced analytics, and GenAI-enabled experiences. This promising future relies heavily on the ability of healthcare leaders to navigate the challenges that threaten to stretch the industry to its limits. Insights from over 50 interviews with key stakeholders—including health systems, insurers, technology vendors, and experts—highlight the pressing need for strategic decision-making that aligns with the Quintuple Aim: improving patient experience, enhancing population health, reducing costs, improving clinician experience, and advancing health equity.
To achieve these goals, healthcare organizations must embrace interoperability and invest in purpose-built technologies that facilitate seamless data sharing across complex systems. By prioritizing collaboration among stakeholders and leveraging innovative solutions, HCOs can transform care delivery and enhance community health outcomes. The path forward requires a commitment to agility and customer obsession, ensuring that healthcare systems are not only responsive to current demands but also resilient in the face of future challenges. The decisions made today will shape the healthcare landscape for years to come, making it imperative for leaders to act decisively and strategically as they prepare for 2030.
FAQs
Healthcare providers should investigate advanced technological solutions to streamline medical processes. Modern digital tools can transform patient care by simplifying administrative tasks, reducing human error, and creating more efficient communication channels. These innovations help medical professionals focus more on direct patient interactions and personalized treatment strategies.
Technology transforms healthcare by empowering systems to examine information, anticipate patient requirements, support medical professionals in identifying conditions, and streamline routine processes, ultimately delivering more tailored treatment experiences that improve overall patient care and operational efficiency.
Modern healthcare software answers now join easily with electronic health record systems, allowing quicker conversation between distinctive health departments. These integrated systems help medical groups percentage patient facts speedy and efficaciously, reducing administrative obstacles and improving typical coordination of healthcare offerings.