Remote Patient Monitoring (RPM) is transforming healthcare delivery in the U.S., leveraging technology to collect & transmit patient-generated health data to healthcare vendors.
The global market for remote patient monitoring was valued at approximately $71.9 billion in 2023 and is projected to grow significantly, reaching around $207.5 billion by 2028. This growth represents a compound annual growth rate (CAGR) of 23.6% during the period from 2023 to 2028.
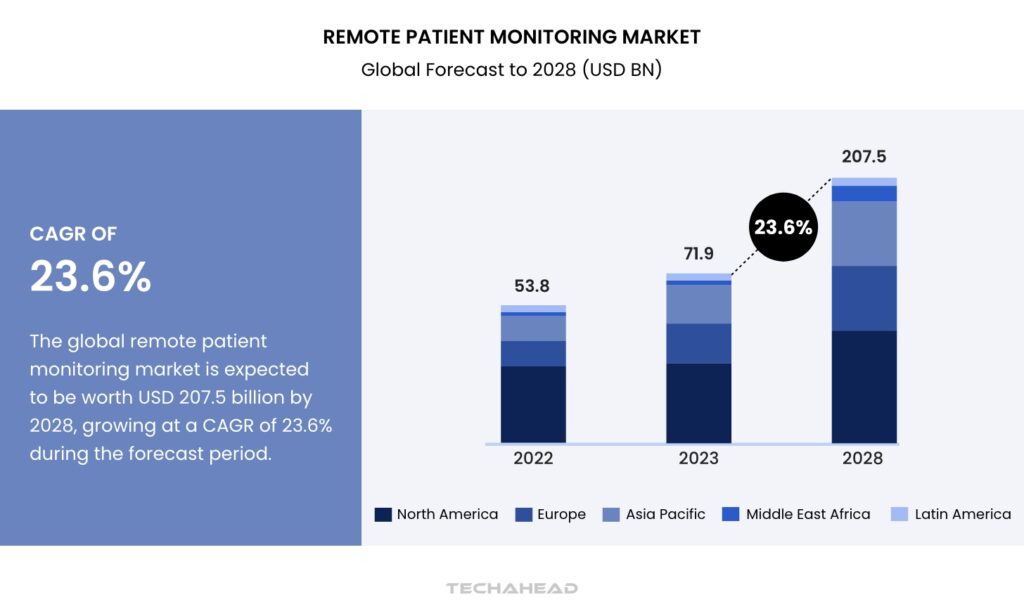
The increasing demand for efficient healthcare solutions and advancements in technology are driving this expansion, highlighting the growing importance of remote monitoring in managing patient health effectively.
The COVID-19 pandemic expanded the adoption of RPM as healthcare structures sought to minimize in-person visits. The Centers for Medicare & Medicaid Services expanded coverage for RPM services, spotting their ability to reduce hospitalizations and improve patient outcomes.
By permitting continuous monitoring, RPM enables identifying health issues early, allowing timely interventions that can prevent emergencies and reduce healthcare costs.
Clinicians who implement RPM programs can enhance care quality while also benefiting financially through improved workflow efficiencies and repayment opportunities.
With the ability to monitor multiple patients simultaneously, RPM now not simplest optimizes scientific resources but additionally empowers patients to take an active role in managing their fitness, ultimately leading to better health results and multiplied patient satisfaction.
How Remote Patient Monitoring Works?
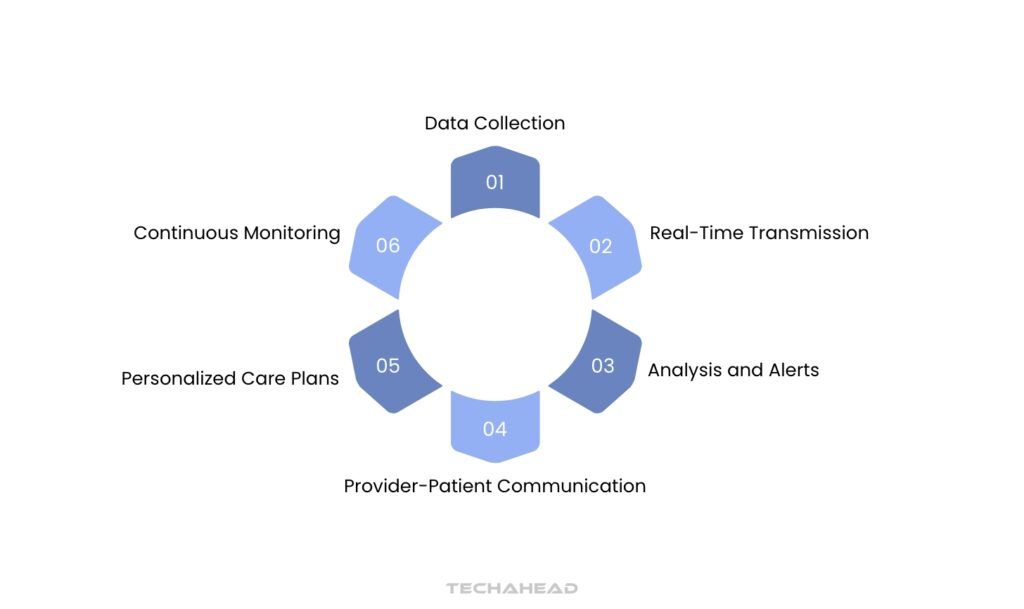
Remote Patient Monitoring (RPM) is revolutionizing healthcare by allowing continuous monitoring of patients’ health through technology. By utilizing wearable devices, along with glucose meters and coronary heart rate monitors, sufferers can track essential signs and symptoms from the comfort of their houses.
This approach not only enhances patient engagement but additionally permits healthcare vendors to accumulate and analyze real-time fitness records, leading to more customized care.
The process begins with patient education on how to use these devices effectively. Understanding the motive and operation of wearables is vital for accurate data collection
Patients are informed about the specific metrics each device tracks, including blood pressure or oxygen levels, and the way to maintain & troubleshoot them. Privacy concerns are also addressed, ensuring patients understand their data is protected under HIPAA regulations.
Once a patient starts using a wearable device, it collects health data through built-in sensors that measure various physiological parameters. This data is then transmitted securely to healthcare providers via Bluetooth or Wi-Fi, ensuring compliance with FDA and HIPAA standards.
With access to this information, providers can intervene as needed. They analyze the data within Electronic Health Records (EHRs) to tailor treatment plans based on individual patient needs. This personalized approach can lead to improved health outcomes and greater patient satisfaction.
Continued patient engagement is vital for the success of RPM programs. Regular feedback and reminders help patients stay involved in their care, fostering a collaborative relationship with healthcare providers. Studies show that RPM can significantly reduce hospital visits and overall healthcare costs while empowering patients to take charge of their health.
The Benefits of Remote Patient Monitoring
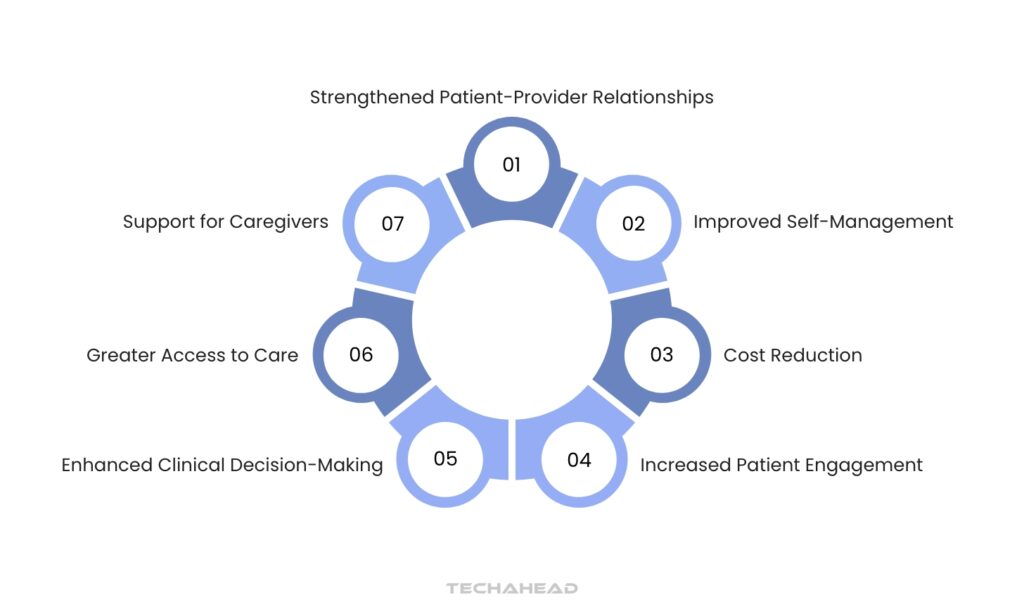
Remote Patient Monitoring (RPM) is a transformative approach in healthcare, offering numerous advantages for patients, providers, payors, and healthcare organizations. Here are seven key benefits of RPM:
Enhanced Clinical Decision-Making
RPM provides healthcare providers with real-time data on patients’ health status between visits. This continuous monitoring allows for timely interventions and adjustments to care plans based on observed trends, ultimately leading to better clinical outcomes.
Improved Self-Management
Patients using RPM tools can actively manage their health conditions with easy-to-use devices tailored to their specific needs. This empowerment fosters adherence to care plans and enhances overall health management, especially for those with chronic conditions.
Cost Reduction
By decreasing unnecessary emergency department visits and hospital admissions, RPM significantly lowers healthcare costs for both payors and providers. It enables earlier interventions and reduces the need for expensive inpatient services.
Increased Patient Engagement
RPM encourages patients to take an active role in their health by providing them with tools and information about their conditions. This engagement leads to better health outcomes as patients become more informed and involved in their care.
Greater Access to Care
RPM breaks down geographical barriers, allowing patients in rural or underserved areas to receive specialized care remotely. This accessibility ensures that more individuals can benefit from timely medical attention without the need for travel.
Strengthened Patient-Provider Relationships
The ongoing communication facilitated by RPM fosters trust and satisfaction between patients and healthcare providers. Patients feel more connected and supported, knowing their providers are monitoring their health closely.
Support for Caregivers
RPM also benefits caregivers by involving them in the care process. Access to patient data allows caregivers to stay informed about their loved ones’ conditions, enhancing collaboration and support in managing health challenges.
The Role of Virtual Care in Healthcare
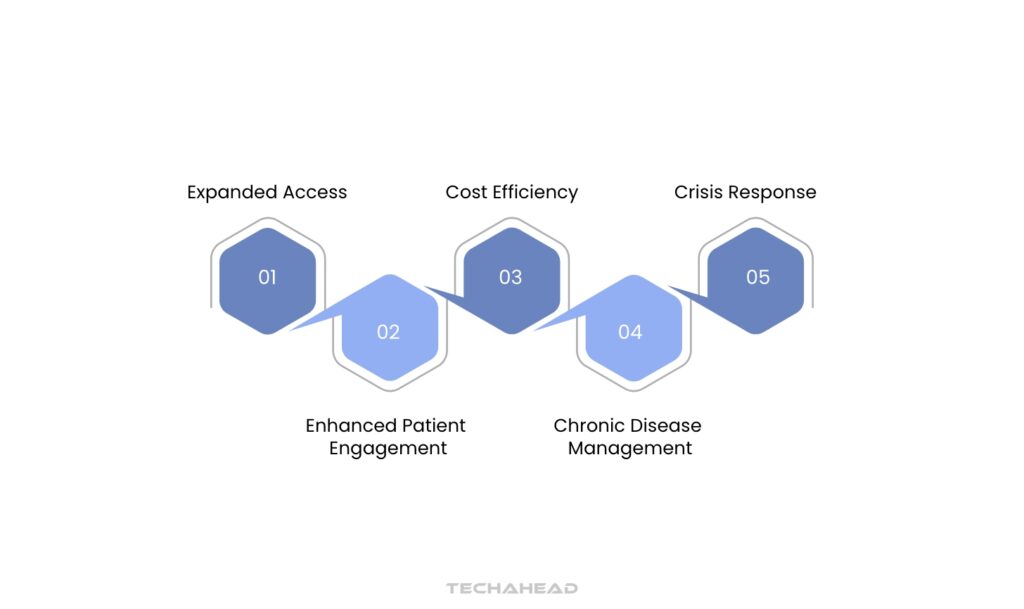
Virtual care has revolutionized the way healthcare is delivered. By leveraging technology, healthcare providers can now connect with patients remotely, offering a wide range of services, from consultations to ongoing care. This shift towards virtual care has numerous benefits, including increased accessibility, improved patient satisfaction, and reduced healthcare costs.
With virtual care, patients can conveniently access healthcare services from the comfort of their homes, eliminating the need for travel and reducing wait times. Telehealth appointments allow for timely consultations, especially for non-urgent conditions, while remote monitoring devices enable continuous tracking of vital signs and other health metrics. Additionally, virtual care can help to reduce the spread of infectious diseases, particularly during outbreaks.
As technology continues to advance, virtual care is poised to become an integral part of the healthcare landscape. By embracing this innovative approach, healthcare providers can deliver high-quality care that is both accessible and affordable.
Challenges & Barriers to Remote Patient Monitoring
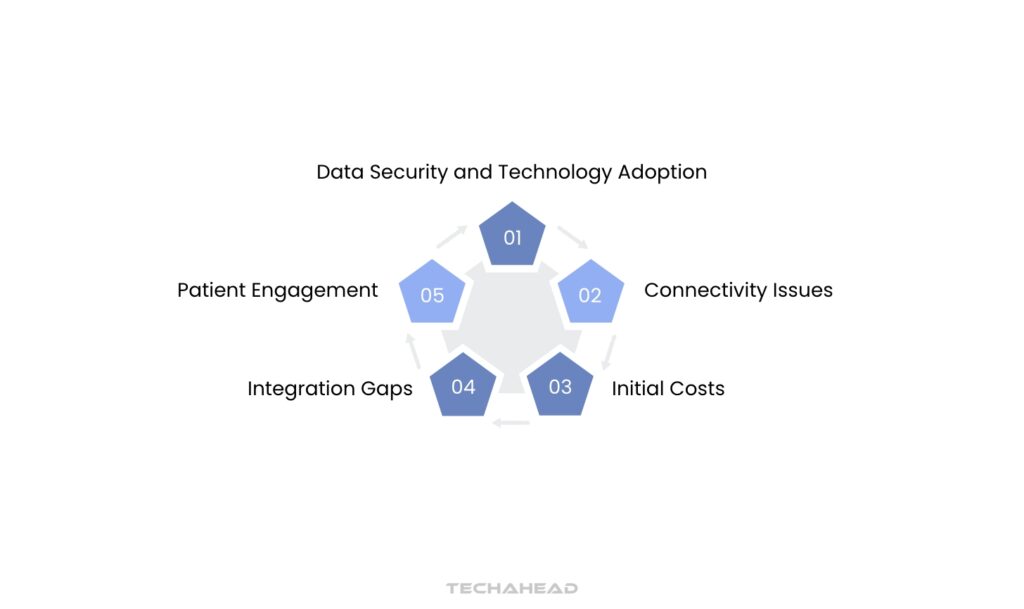
Remote patient monitoring (RPM) holds immense potential for improving patient care and reducing healthcare costs. However, its widespread adoption faces several challenges and barriers.
One significant challenge is the digital divide, where access to reliable internet connectivity and technological devices remains limited for many patients. This can hinder the effective implementation of RPM programs, particularly in rural and underserved areas.
Another hurdle is the lack of standardized data formats and interoperability between different healthcare systems. This can make it difficult to share and analyze patient data, hindering the development of comprehensive and personalized care plans.
Privacy and security concerns are also paramount. Protecting sensitive patient data is essential, and robust security measures must be implemented to mitigate risks.
Furthermore, reimbursement challenges can hinder the adoption of RPM programs. Healthcare providers may face difficulties in receiving adequate reimbursement for remote monitoring services from insurance providers.
Lastly, there’s a need for ongoing education and training for both healthcare providers and patients to effectively utilize RPM technologies. This includes educating patients on how to use devices, collect data, and share information with their healthcare providers.
Despite these challenges, the potential benefits of RPM are undeniable. By addressing these barriers and investing in technological advancements, we can unlock the full potential of remote patient monitoring and improve the quality of care for patients worldwide.
Remote Patient Monitoring for Chronic Disease Management
Imagine Sarah, a 58-year-old diabetic patient who struggles to manage her condition while maintaining an active lifestyle. Traditional healthcare often meant periodic clinic visits and uncertainty between appointments. Today, remote patient monitoring (RPM) is revolutionizing how patients like Sarah interact with healthcare.
Modern wearable devices have transformed chronic disease management from reactive to proactive. These smart devices continuously track vital signs, providing real-time insights into a patient’s health status. For individuals managing conditions like diabetes, heart disease, or respiratory disorders, this means unprecedented levels of personalized care.
The technology works through sophisticated sensors integrated into wearable devices – from smartwatches monitoring heart rates to patch biosensors tracking body temperature and movement. These devices collect comprehensive physiological data, which is then securely transmitted to healthcare providers through cloud platforms. Doctors can now access detailed health information, enabling them to detect potential complications early and adjust treatment plans precisely.
Consider the impact for patients with chronic conditions. A sudden change in heart rate, irregular breathing, or unexpected body temperature can trigger immediate medical alerts. This continuous monitoring reduces hospital readmissions and empowers patients to take control of their health journey..
For patients like Sarah, remote monitoring means more than just data collection. It represents hope – the ability to live fuller, more confident lives while maintaining close medical supervision. As technology advances, the future of chronic disease management looks increasingly personalized, preventive, and patient-centric.
Virtual Care for Mental Health and Behavioral Health

The rise of virtual care for mental health & behavioral health has transformed the landscape of healthcare delivery, particularly in the wake of the COVID-19 pandemic.
This shift to telehealth has made accessing mental health services more convenient, allowing individuals to seek help from the comfort of their homes.
With nearly 57.8 million American adults diagnosed with behavioral health conditions, the need for accessible care has never been more critical. Unfortunately, only about 43% of those individuals receive any form of treatment, highlighting a significant gap in care availability.
Virtual care offers a solution to many barriers that prevent individuals from seeking help, such as stigma, transportation issues, and the time constraints associated with traditional in-person visits.
According to recent studies, telehealth accounted for 62.5% of mental health diagnoses in December 2022, indicating a substantial reliance on virtual platforms for mental health support.
This trend is particularly beneficial for populations in rural areas or those with mobility challenges, as it enables them to connect with licensed professionals without the need for travel.
Moreover, virtual care has proven effective in delivering quality mental health services. Research indicates that teletherapy can yield comparable outcomes to in-person sessions, especially for conditions like anxiety and depression.
Patients report high satisfaction levels with virtual interactions, often finding it easier to establish therapeutic relationships with their providers through digital platforms.
To maximize the benefits of virtual mental health care, individuals should consider their preferences and needs when choosing a service. They might ask themselves whether they prefer video consultations or self-directed healthcare mobile apps for managing their mental health.
Engaging with primary care physicians can also provide valuable guidance on available resources and potential referrals to virtual therapists.
As the healthcare system continues to adapt to these changes, it is essential for patients to remain informed about their options. Insurance providers are increasingly covering virtual therapy sessions, making this mode of care not only accessible but also affordable.
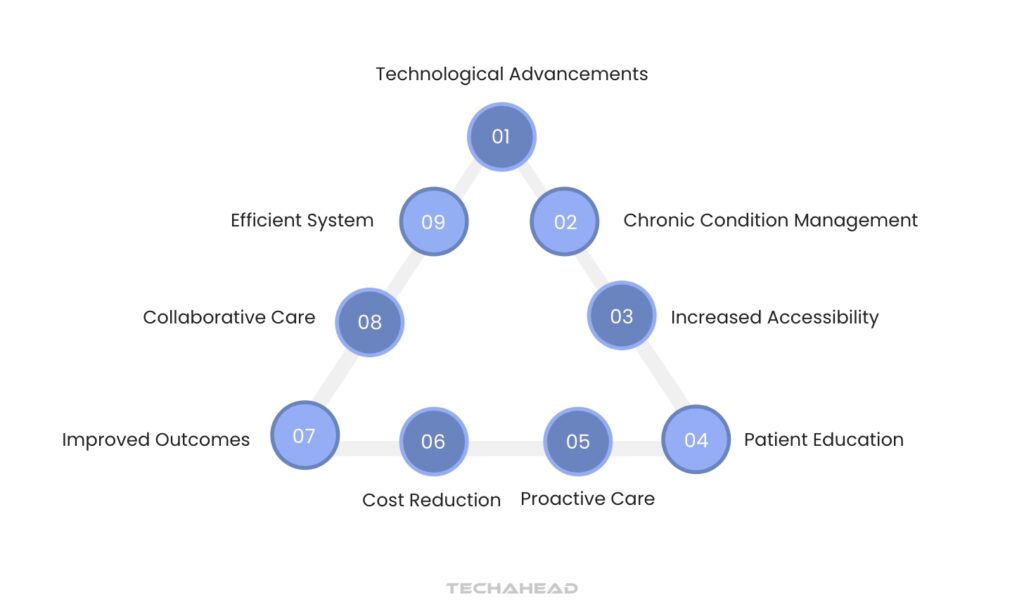
The Future of Remote Patient Monitoring and Virtual Care
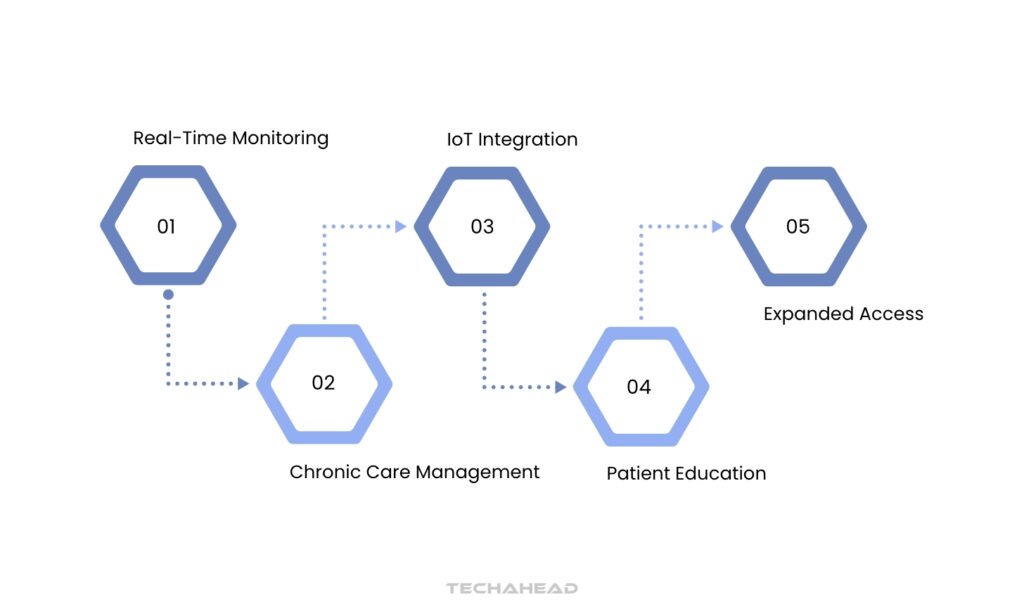
The future of remote patient monitoring (RPM) & virtual care is poised for significant advancements, driven by technological innovations and changing patient needs. RPM utilizes technology to continuously monitor patients’ health, allowing healthcare providers to track vital signs and health metrics in real-time.
This capability is particularly beneficial for managing chronic conditions, as it enables timely interventions and personalized treatment plans. With the integration of Internet of Things (IoT) devices and electronic health records (EHR), healthcare professionals can gain comprehensive insights into a patient’s health status, fostering a more proactive approach to care.
Education plays a crucial role in the successful implementation of RPM. Patients need to understand how to use wearable devices effectively, which can include everything from blood pressure monitors to ECG sensors.
Ensuring that patients are well-informed about these technologies not only enhances data accuracy but also boosts their confidence in managing their health remotely. Moreover, as telehealth becomes increasingly accepted, insurance coverage for virtual services is expanding, making RPM more accessible to a broader population.
The potential for reduced hospitalizations and healthcare costs further underscores the value of RPM. Studies indicate that patients engaged in RPM experience fewer emergency visits and improved overall health outcomes.
As healthcare continues to evolve, the collaboration between patients and providers will be essential in maximizing the benefits of remote monitoring and virtual care, leading to a more efficient and effective healthcare system.
How to Implement Remote Patient Monitoring in Your Healthcare Practice
The future of remote patient monitoring (RPM) and virtual care is poised for significant advancements, driven by technological innovations and changing patient needs. RPM utilizes technology to continuously monitor patients’ health, allowing healthcare providers to track vital signs and health metrics in real-time.
This capability is particularly beneficial for managing chronic conditions, as it enables timely interventions and personalized treatment plans. With the integration of Internet of Things (IoT) devices and electronic health records (EHR), healthcare professionals can gain comprehensive insights into a patient’s health status, fostering a more proactive approach to care.
Education plays a crucial role in the successful implementation of RPM. Patients need to understand how to use wearable devices effectively, which can include everything from blood pressure monitors to ECG sensors.
Ensuring that patients are well-informed about these technologies not only enhances data accuracy but also boosts their confidence in managing their health remotely. Moreover, as telehealth becomes increasingly accepted, insurance coverage for virtual services is expanding, making RPM more accessible to a broader population.
The potential for reduced hospitalizations and healthcare costs further underscores the value of RPM. Studies indicate that patients engaged in RPM experience fewer emergency visits and improved overall health outcomes.
As healthcare continues to evolve, the collaboration between patients and providers will be essential in maximizing the benefits of remote monitoring and virtual care, leading to a more efficient and effective healthcare system.
Conclusion
In conclusion, remote patient monitoring and virtual care are reshaping the future of healthcare delivery. By leveraging technology, these approaches enhance patient engagement and provide continuous, personalized care, especially for those managing chronic conditions. The integration of wearable devices allows for real-time health data collection, enabling healthcare providers to make informed decisions and timely interventions.
As patients become more educated about these technologies, their comfort and confidence in using them will grow, leading to better health outcomes. Ultimately, the collaboration between patients and healthcare providers is essential for maximizing the benefits of remote monitoring and ensuring a more efficient healthcare system.
You can even reach out to an experienced professional who has worked in developing a remote patient monitoring application, like TechAhead. So Contact us to understand better your needs for your project. Our professionals will serve you justice with our healthcare app development services.
FAQs
Remote patient monitoring cuts healthcare expenses by preventing unnecessary hospital trips and allowing early, proactive medical intervention.
Doctors recommend checking this regularly, usually daily, based on your specific health needs and their personalized guidance.
More patients use virtual doctor visits, smart health devices gain popularity, and people prioritize staying healthy before getting sick.
Remote monitoring can catch health warning signs early, helping doctors intervene before problems worsen and potentially prevent serious complications.
Multiple devices now effortlessly monitor diverse health indicators in real-time, providing comprehensive wellness insights across various medical conditions.